Preschoolers and ADHD
Recommended treatment for children under 5 is behavioral therapy, not stimulant medication
While ADHD is most often diagnosed in school-aged children, it can be diagnosed in children as young as three.
Of course we expect all preschoolers to be active — more inclined to run around than to sit still. And we expect them to be impulsive — prone to doing things without thinking about the consequences. But some kids are extemely active — parents typically describe them as “bouncing off the walls” — and they’re so impulsive they’re extraordinarily difficult to manage.
These children may have ADHD, and early diagnosis and treatment can help them rein in impulsive behavior that’s causing problems for them, and their families. They can get along better with other kids and be able to participate in activities appropriate for their age. But it’s important to know that the recommended first-line treatment for preschoolers with ADHD is different from what’s recommended for older kids.
ADHD experts and the American Academy of Pediatrics agree that behavioral therapy is the preferred treatment for preschoolers with ADHD, and that stimulant medication should be considered only if behavioral therapy isn’t available or hasn’t worked. It can also also be considered if the child or the family is at risk of serious harm.
How is ADHD diagnosed in preschoolers?
It is usually hyperactive and impulsive behavior that leads to an ADHD diagnosis in preschoolers. They may have been kicked out of preschool or banned from playdates. Their parents worry constantly that they will run into the street or hurt themselves in some other impulsive way.
From 2 to 6 percent of preschoolers are estimated to have the disorder — a much lower percentage than school age kids. Boys are twice as likely as girls to be diagnosed.
Mark Stein, the director of the ADHD and Related Disorders Program (PEARL Clinic) at Seattle Children’s Hospital, explains that behavioral problems are usually what cause parents to bring preschoolers in for evaluation. He notes that one of the screening questions he uses when taking a child’s history is “What percentage of the time, when you give your child a command, do they obey you within five seconds?” By age four, he says, it should be 75 to 80 percent. “In my patients it’s like 10 percent.”
But Dr. Stein, who is also a professor of psychiatry and behavioral science at the University of Washington, emphasizes that diagnosing ADHD at this age should be done with great care, since all preschool children exhibit some hyperactivity, impulsivity and inattention, the key symptoms of ADHD.
Observing a child’s behavior in the doctor’s office is not sufficient for a diagnosis, as symptoms may not be present in that environment. Pediatricians are encouraged to collect screening questionnaires filled out not only by a parent but by at least one other adult who spends time with the child. Symptoms must be present in more than one setting — ie at home, at preschool or daycare, with relatives or family friends.
As Dr. Stein notes, it’s harder to evaluate children who are not yet in a structured environment like preschool, where their behavior is easer to observe and compare to that of other kids.
Dr. Andrew Adesman, a pediatrician who is Chief of Developmental & Behavioral Pediatrics at Cohen Children’s Medical Center of New York, adds that for kids who have been kept at home, if parents are frustrated with their behavior and suspect ADHD, sending them to preschool or daycare can be a good way to get some validation, as well as some respite. “Parents know their child best, but they don’t have the training, experience and perspective on what’s typical at a certain age,” he explains.
Dr. Stein notes that it’s the diagnostician’s job to rule out other conditions that look like ADHD. “There are medical mimics, like hypothyroidism, and poor sleep problems and medication effects. And there are psychiatric mimics, like having autism or depression or anxiety.”
Behavioral treatment for ADHD
Parent training for behavioral management techniques is the recommended treatment for preschoolers with ADHD. Through these programs, parents learn how to more effectively shape the behavior of young children, and the children usually show marked improvement in their ability to comply with direction and rein in their impulsivity.
Why parent training, rather than therapy delivered directly to the child? Dr. Adesman explains that children are often referred for play therapy, but this is not a very helpful intervention for ADHD. “At its worst it’s like an expensive play date. At its best it’s a well-intentioned intervention that doesn’t have any evidence to support it.” What families should be pursuing is parent training in behavior management techniques.
“Intuitively one would think that if the child has the problem, the therapy should be focued on the child. The reality is that, while it’s the child who has the problem, what we want to do is change the environment so we can set the child up for success. And that typically involves working with parents and teachers,” he explains. “If a child has allergies — the problem is with the child but the solution is in working with the environment. You might get rid of the carpet or the drapes or find a new home for the cat. We can do things with the environment to help kids behave better.”
These programs teach parents how to use praise, or positive reinforcement, to promote the behaviors they want to encourage. And parents are taught to deliver consistent consequences when kids don’t comply. The result is that kids learn to modulate their behavior to meet expectations and the family conflict can be reduced, sometimes dramatically.
Programs that have shown evidence of effectiveness include:
- Parent-Child Interaction Therapy (PCIT)
- Parent Management Training (PMT)
- Positive Parenting Program (Triple P)
- The Incredible Years
Dr. Stein notes that the preschool years are the “sweet spot” for parent training, when evidence shows that it can have the most effect. “I always tell parents, you know, now is the ideal time. You don’t want to be dealing with a noncompliant 15- or 16-year-old.”
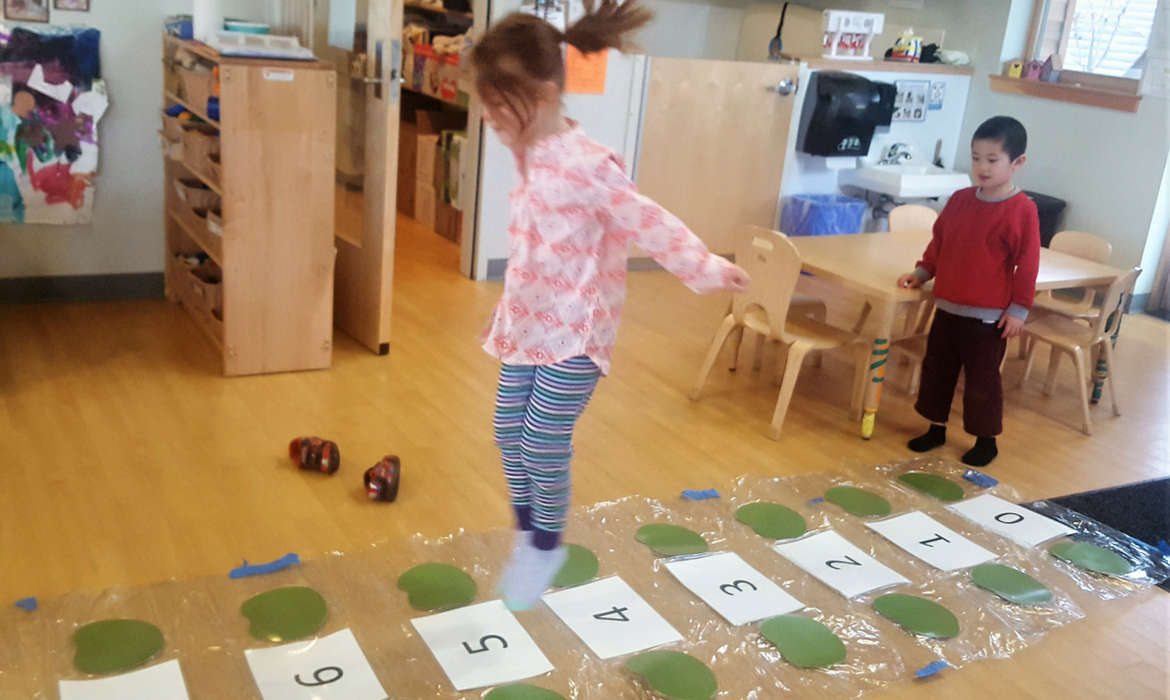
Dr. Stein also recommends that parents of preschoolers with ADHD get them into a structured school setting. When kids have behavior problems, parents often take them out of preschool, but they really need to get them more in.
If children can’t behave well enough for a mainstream preschool, there are special preschools for children with behavioral problems. “The idea is to not run away from structure, but to get more intensive services. The parents need the respite, and the kids need to learn to be socialized.”
Dr. Adesman adds that it’s especially important that these children have some experience of meeting expectations in a structured setting before they go to kindergarten.
When should medication be considered?
In general, stimulant medication should be considered only for preschoolers who haven’t been helped by behavior therapy, or whose behavior is so severe that it’s dangerous or it’s severely impacting their lives, and their families’ lives.
One reason to try behavior therapy first is that while stimulant meds are very effective for most school-aged children — the response rate is more than 70 percent — Dr. Adeson notes that in preschoolers the response rate drops to 50 percent.
Dr. Adesman offers this list, based on recommendations of the AAP, of situations in which medication might be an appropriate choice:
- Behavior therapy has been unsuccessful
- Significant risk of injury to the child
- Significant risk of injury to other children or caregivers
- Ejection from preschool or daycare
- Threatened ejection from preschool or daycare
- Strong family history of ADHD
- Possible central nervous system injury, such as prematurity, prenatal alcohol or cocaine exposure, or lead poisoning
- ADHD symptoms interfere with other needed therapy, such as speech/language, OT, PT
- Parent or guardian on the verge of a “mental breakdown” because of the child’s behavior
- Marriage on the verge of divorce or separation because of the child’s behavior
Prescribing to preschoolers can be confusing because there is a discrepancy between what is approved by the FDA and what is recommended by the AAP.
Of the two types of stimulant medication — those based on methylphenidate and those based on amphetamine — the FDA has approved only short-acting amphetamine-based medications (Dexedrine and Adderall) for children 3-5. The AAP, on the other hand, based on the results of the Preschool ADHD Treatment Study (PATS) that used mepthylphenidate, recommends methylphenidate-based medications for children 4-5.
A reasonable approach, Dr. Adesman adds, would be to use a methlyphenedate medication first, and if it’s not working, try amphetamine-based.
What everyone agrees on is that if medication is used it should be an extremely low dose. And the good news here is that there are new formulations for preschoolers that not only don’t require swallowing a pill, but they can deliver very small doses — “liquids that can be titrated down, or a patch that can be cut in half,” he explained.
Behavior training for preschoolers
But Dr. Adesman stresses that medication should be considered only if parent training isn’t working well enough, or if the situation is extreme.
“Children don’t have ADHD because their parents are ineffective. But they can definitely be part of the solution,” he said.
And one of the best things about parent training is that it helps kids whether or not they have an ADHD diagnosis, so there is no downside to trying it if kids are having behavior problems. “If there are behavioral challenges, with or without an ADHD diagnosis, parents should get training,” he said. “It will help the child, it will help the parents, and it will help the other kids in the family, too.“
What to Do (and Not Do) When Children Are Anxious by Clark Goldstein, PhD
What Is Separation Anxiety? by Rachel Ehmke
Tips for Calming Anxious Kids by Michaela Searfoorce
How to Foster Resilience in Kids by Alan Ravitz, MD, MS
Nonverbal communication: body language and tone of voice by Raising Children Network (Australia) Limited.
The Other Senses: Interoception by Pat Porter
Dyslexia – in tune but out of time by Usha Goswami
Side Effects of ADHD Medication by Roy Boorady, MD
Autism spectrum disorder (ASD) by Mayo Clinic Staff
Mental illness in children: Know the signs by Mayo Clinic Staff
6 Types of Anxiety that Can Affect Children by Kathleen Smith, PhD, LPC
What Is a Language Processing Disorder? by Devon Frye